Life in the Box: Breath and Covid-19: Part Two

Having looked into questions about why and how to wear a mask and what kind of mask to make in Part One, now I turn to environmental studies to better my odds of not getting Covid-19.
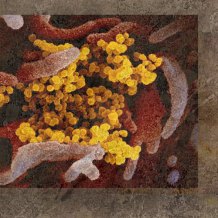
How much Covid do you have to breathe in to get sick?
I wondered if the number of Covid particles you breathe in has an effect on whether Covid actually lodges in your body enough to make you sick. The answer is: nobody knows how much virus it takes to harm a human body. However, it makes sense to get as little exposure to the virus as possible.
The particles can float invisibly in the air, so you don’t know how much Covid is there. You don’t always see the person who coughed or sneezed out the virus, especially if they were there 3 hours ago. There aren’t little virus monitors that can tell you this, either. (Wouldn’t that be a great cell phone app?)
Unfortunately, the only way to assess how much Covid is in the air is to guess, based on how crowded the space is and how good the air circulation is. Outside settings are better at dispersing particles than closed indoor spaces are.
One study looked at air quality in hospitals and other indoor settings, using aerosol traps that caught samples and counted the genetic material of Covid (RNA.)
It seems bathrooms are trouble spots, due to them having bad air circulation and being a place where body fluids are exposed to air. Covid can come out in poop and pee, and go aerial when you flush. I’ll say more about this in the “bathroom section.”
But here’s a slight side note: even though there is RNA of Covid present, it might not be viable—in other words it might not be alive enough to harm anyone. More studies are needed.
At this point, I think it’s wise to assume the less Covid RNA we are ingesting, the better.
Super Spreaders
Another confusing part of this is that some people exhale large concentrations of the virus in their breath—scientists are calling these people “super spreaders.” Some of these super spreaders, despite the large amount of virus they carry, have no symptoms of the virus at all. That doesn’t mean the people they infect will be symptom free. A researcher in London reports that only 10% of the people are spreading 80% of the disease.
Some people shed far more virus, and for a longer period of time, than others, perhaps because of differences in their immune system or the distribution of virus receptors in their body.
After South Korea relaxed social distancing rules in early May, a man who later tested positive for COVID-19 visited several clubs in Seoul; public health officials scrambled to identify thousands of potential contacts and have already found 170 new cases.

However, most people with Covid are only able to spread the virus for a short period of time.
Emerging evidence suggests COVID-19 patients are most infectious for a short period of time. Entering a high-risk setting in that period may touch off a superspreading event, Kucharski says; “Two days later, that person could behave in the same way and you wouldn’t see the same outcome.”
On the other hand, the virus isn’t just spread by breath: it can come out the “other end,” too.
Researchers have found that the new coronavirus, [Covid-19] can be shed in feces for up to a month after the illness. That’s longer than in respiratory samples, though how much of that time the virus could be causing infections and whether the virus has infected humans through fecal waste isn’t yet known. PBS Newshour Link
The reassuring part of this is that if you find you have been near someone who later tests positive, you have a pretty good chance of not getting it from them. Of course, if you were both wearing masks, that makes your odds even better. However, be careful who you kiss.
The virus may be shed in saliva, semen, and feces; whether it is shed in vaginal fluids isn’t known. Kissing can transmit the virus. Transmission of the virus through feces, or during vaginal or anal intercourse or oral sex, appears to be extremely unlikely at this time. [note: See “Bathroom” section.] Harvard Health Link

Don’t Shout or Sing
People who speak loudly, shout or sing (without masks) seem to infect clusters of others. It seems to me that this is the “velocity” aspect, as well as the large breaths they take that can increase the number of droplets they expel, as well as the distance the droplets carry.
Anecdotally, outbreaks prior to social distancing were more common in loud exercise classes than in quiet ones.
…although Zumba classes have been connected to outbreaks, Pilates classes, which are not as intense, have not, Knight notes. “Maybe slow, gentle breathing is not a risk factor, but heavy, deep, or rapid breathing and shouting is.” Science Magazine Link 2

How Particles Move
There are some great illustrations online of how the particles we exhale move around us. The first minute of this Vox video shows how people sitting 14 feet apart inside a restaurant have contracted Covid. Later, about 3 minutes in, the video illustrates how particles spread differently depending on if they are sprayed outside or inside.
Vox video about Particles Spread – On YouTube
Another fun fact is that if you are running or riding a bicycle outdoors with someone else, you will be less likely to contract the disease from each other if you are side-by-side, not single file. This is because your breath trails behind you in a “slipstream.” I also noticed that the further away you are, the lower (closer to the ground) it moves. So one would assume it’s less easy to inhale there.
Illustrations of slipstream by Eindhoven University of Technology, Netherlands. Reported by China Government’s European Network which is rated “mixed” credibility. However, the illustrations check out from the Eindhoven website. CGEN Video about Biking and Running and Covid
There is a lot of research that says Covid is much easier to contract indoors than outdoors. I’m wondering if there are ways for us to change our inside environments to lower the spread.
Humidity
I found a few interesting articles about how humidity can lessen the effectiveness of Covid spread.
In general, it’s thought that dry inside air is a contributing factor in the increase in flu and virus infections in the winter months when indoor air is drier, so that can apply to Covid. It might be worth it to check your indoor humidity and use a humidifier in the winter.
Science Daily article about humidity and Covid
One Harvard study found that Covid doesn’t live as long in a hot and humid laboratory setting, but heat and humidity might not be the only factors. Also, Covid has been spreading in hot and humid climates (as well as cold and dry climates.)
The report found that in laboratory settings, higher temperatures and higher levels of humidity decreased survival of the COVID-19 coronavirus. However, studies looking at viral spread in varying climate conditions in the natural environment had inconsistent results.
The researchers concluded that conditions of increased heat and humidity alone may not significantly slow the spread of the COVID-19 virus. Harvard Health Article about Humidity
One other factor is not really intuitive: human lungs can work better in humid conditions. In my experience, it seems harder to breathe in humid conditions, but this Yale video says that the little hairs (cilia) in our lungs are more active in cleaning out our lungs (clearing out particles like Covid) in higher humidity.
Yale Video about Cilia and Winter Flu Mortality
Want to see a short movie of cilia waving?
Air Pressure
When the Army Corps of Engineers set up temporary hospital facilities for Covid patient overflow earlier this year, they included portable machines that would create negative air pressure in the patients’ rooms, basically causing the air to be pulled down a drain. In order for this to work, the rooms had to be sealed off. Theoretically, this could be done in larger areas, like hospital wards or office spaces. I haven’t yet found any examples of this being done for those larger spaces.
Science Daily article about an experiment in creating negative air pressure
Air Purifiers
Consumer Reports looked into the use of air purifiers against Covid. Their researchers believe that air purifiers can help reduce the particulates that hold the virus if used in, say, a Covid patient’s room. It’s better than nothing, but opening windows is cheaper and more effective.
Consumer Reports article on air purifiers
Why 6 feet?
So, the distance of 6 feet is apparently chosen for how far away you need to stand from someone in while talking in a normal conversation.
The bad news is that our exhalations often travel further than 6 feet, and maybe double that.
Article about how far exhalations travel
The earlier example in a Chinese restaurant showed that Covid was spread 14 feet away by the air conditioning unit. Weirdly in that example, not everyone within that 14-foot range caught the infection. Who knows why? But half of them did get Covid. That’s pretty bad odds. And, because it’s nearly impossible to wear a mask while eating and drinking, I’m still wary of going to a restaurant and eating inside.
Another factor in restaurants and grocery stores is: you can’t control who was in a room three hours before you arrived, and you can’t control the idiots who pass too close to you without wearing masks.
And, yes, if someone sneezes or coughs in another aisle (without a mask,) it can leap over the shelves towards you.
Video illustration of germs jumping over shelves
Since there’s nothing you can do about floating particles, the best thing you can do besides wear a mask and wash your hands, according Vox reports, is to limit the time you spend in potentially troublesome environments. And speaking of troublesome, here’s that new information about bathrooms.
Bathrooms

Did you know that flushing a toilet can spread germs? Now we’re hearing that putting down the lid is a health measure we can all take, if we are in a bathroom where they have lids. (Oh, and wash your hands, definitely!)
PBS NewsHour: A study on hospital bathrooms found that the amount of those particles spiked after a toilet was flushed, and the concentration in the air remained high 30 minutes later. It didn’t matter if the test was done right next to the toilet or 3 feet away. Second and third flushes continued to spread particles. Another study, published June 16, simulated toilet plumes from flushing and also found that a large number of particles rose above the toilet seat and lingered in the air.
The scientists’ advice: close the lid before flushing… When you’re done, thoroughly wash your hands with soap and water, and maybe skip the hot-air hand dryer, which can also create aerosols and blow them toward you. PBS Newshour article about bathrooms
Washington Post article about Toilet Plumes
Covid from body fluids found on hotel surfaces, bedsheets, etc: Study advises care when cleaning all living spaces around Covid patients.
Conclusion:
After reading and studying what we know so far, I will be continuing to wear a mask, wash my hands often, stay out of crowds, and spend as little time as possible in public restrooms. (I wonder how long I can hold my breath in there?! )
I will still only venture into shops for as little time as possible, and keep physically distant as much as possible. I will wear a mask at the drive-through window to protect the workers and keep using hand sanitizer in the car after handling money and products.
However, I will not eat inside at restaurants. I will go inside them for a quick carry-out order, but will be wearing a mask and washing up soon thereafter.
I will continue to enjoy walks in parks where I seldom come close to others. I will either wear a mask or have one in my pocket to slip on quickly if non-mask-wearers appear suddenly.
I will also continue to enjoy occasional gatherings of friends outside—asking them to stay distant and wear masks. Maybe 12 feet, not 6. We tend to laugh a lot! (Velocity!)
I have purchased a plastic face shield, but haven’t used it yet. I’m thinking it’s a good idea, but am shy about looking “different” and having to explain it. I will attempt to get over that.
Because of the videos, I can now envision a cloud of exhalations around myself and others. This flurry of research has helped me feel less confused. Even though we don’t know everything about the virus, we do have some good inklings of how to beat the odds for now.

Nancy Heather Brown is a retired, Emmy Award-winning television producer whose career has included interviewing, writing, narrating and editing for a span of four decades. Today, she enjoys learning new things and reflecting upon the creative process and life issues, both inside and outside the box. Her opinions are her own, and are not necessarily those of this web site.
Note: This research was performed the week of June 22,2020. Hopefully, there will be new science and our understanding will expand and change.
Fact Check: The research was fact-checked on Media Bias/Fact Check
Summary page of recent Covid-related research from Nature
Washington Post Live Updates page with Coronavirus Headlines
AARP article on safe grocery shopping
World Health Organization Covid Myth Busters
How to talk about Covid before socializing with friends
September Update on Public Restrooms from AARP





Leave a Reply